Fat Cell Study Shows Advancing Treatments for Obesity, Diabetes - Penn Medicine
05/31/2023
Findings represent the first structural details of uncoupling protein 1 (UCP1), which allows fat tissue to burn off calories as heat
PHILADELPHIA—New research has unlocked insights into how “good fat” tissue could potentially be harnessed to combat obesity and remove glucose from the blood, helping to control diabetes. Published today in Science Advances, the work is a collaboration between researchers with the Perelman School of Medicine at the University of Pennsylvania and University of Cambridge, Free University of Brussels and University of East Anglia.
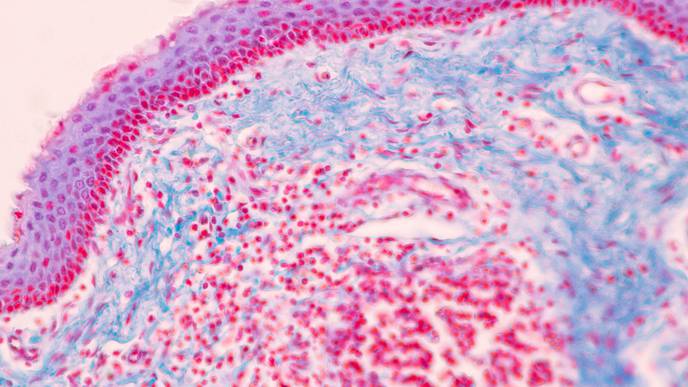
Human bodies consist of two types of fat: brown and white. Brown fat breaks down blood sugar (glucose) and fat molecules, generating heat in response to cold temperatures helping to maintain normal body temperature. The majority of fat in humans is white fat, and building up too much white fat contributes to obesity and other health issues.
Using the Krios G3i, a cryogenic electron microscope at the Penn Singh Center for Nanotechnology researchers were able to view mitochondrial uncoupling protein 1 (UCP1)—a protein which allows fat tissue to burn off calories as heat—in atomic detail for the first time. This work uncovered new insights into how this protein’s activity in brown fat cells could potentially be harnessed for weight loss.
“This is an exciting development that follows more than four decades of research into what UCP1 looks like and how it works,” said Vera Moiseenkova-Bell, PhD, a professor of Systems Pharmacology and Translational Therapeutics and faculty director of the Beckman Center for Cryo-Electron Microscopy. “These new indings would not have been possible without the collaboration between everyone involved.”
In mammals, UCP1 gives brown fat a specialized ability to burn calories as heat for maintaining a stable body temperature. When activated by fatty acids, UCP1 short-circuits the mitochondria—known as the powerhouse of the cell for its work releasing energy from food—by allowing protons to seep across mitochondrial inner membrane. The short-circuiting generates heat and allowing the body to regulate its temperature through a process called thermogenesis.
This work was supported by the Medical Research Council (MC_UU_00028/2, MC_UU_00015/1), by the U.K. Biological and Biotechnological Sciences Research Council (BB/S00940X/1) and by National Institutes of Health/National Institute of General Medical Sciences (R01 GM073791, F31 HL156431). Nanobody discovery was funded by the Instruct-ERIC part of the European Strategy Forum on Research infrastructures, and the Research Foundation – Flanders, and the Strategic Research Program of the Vrije Universiteit Brussel.
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation’s first medical school) and the University of Pennsylvania Health System, which together form a $9.9 billion enterprise.
The Perelman School of Medicine has been ranked among the top medical schools in the United States for more than 20 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $546 million awarded in the 2021 fiscal year.
The University of Pennsylvania Health System’s patient care facilities include: the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center—which are recognized as one of the nation’s top “Honor Roll” hospitals by U.S. News & World Report—Chester County Hospital; Lancaster General Health; Penn Medicine Princeton Health; and Pennsylvania Hospital, the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is powered by a talented and dedicated workforce of more than 47,000 people. The organization also has alliances with top community health systems across both Southeastern Pennsylvania and Southern New Jersey, creating more options for patients no matter where they live.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2021, Penn Medicine provided more than $619 million to benefit our community.

Facebook Comments